Radiculopathy: What is it and what can I do about it?

Radiculopathy is a set of neurological conditions that occur when there is a compression of nerve roots in the spine (5). The location of symptoms is dependent upon which nerve root is affected along the spinal cord (5). The two types of radiculopathy Cervical and Lumbar are both typically caused by disc related pathologies such as herniation or prolapse (bulging disc). However, radiculopathy can also be induced by bone spurs, trauma, osteoarthritis, inflammation, tumour or diabetes – albeit these causes are much less common. Risk factors for radiculopathy include:
- Age
- Race
- Hereditary factors
- Poor posture
- Spinal abnormalities
- Occupations involving heavy labour, sports or military service
Cervical Radiculopathy
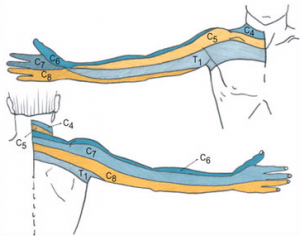
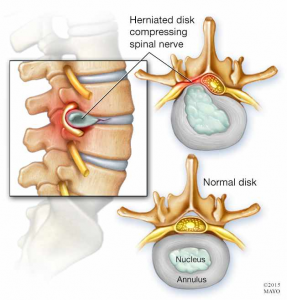
Cervical radiculopathy is a type of radiculopathy that leads to pain locally in the neck and often pain, pins or needles that radiates into your shoulder and/or arm. Typically, the discs in the neck can become problematic following a violent movement of the head, spending too long in a certain neck position or can come on for no apparent reason. These discs sit between each vertebra and are important for shock absorption and movement. They are filled with fluid called nucleus pulposus and when a disc injury occurs, this fluid can potentially protrude or prolapse (herniate) toward the nerve roots that run behind them. This in turn, causes the nerve roots to send pain or alternate sensations down the area that the nerve root innervates. Where you experience your symptoms depends upon which level the disc is injured at and therefore which nerve root is affected.
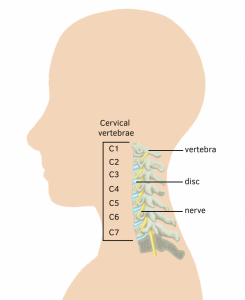
If you are experiencing symptoms such as this, seeing a health professional for a thorough and accurate diagnosis is paramount.
Lumbar radiculopathy
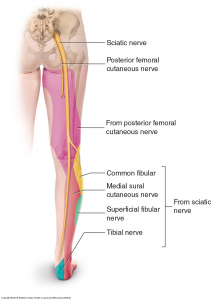
Similar injuries also occur in the lumbar spine (lower back). Once again, the primary causation due to a disc and nerve root pathology – both causes and management of this type of injury have comparisons. Similarly to the upper limb, the distribution of your symptoms is dependant upon which spinal level the disc is injured or inflamed. Most commonly, lumbar radiculopathy results in symptoms that run down the back of your thigh and/or into the knee, calf and foot.
Disc related pathologies that cause these symptoms take, on average, 4-6 weeks to heal depending on age, injury background, rest, etc. However, during this time there are things you can do and others can do to help reduce the unwanted symptoms that persist while the injury heals.
What YOU can do:
- Rest
- like with any injury, particularly in the early or acute stages (typically weeks 1-2) it is important to give your neck a rest. Reducing movements that bring on your pain or sensation down your arm(s) is important during this stage to prevent further damage.
- Non-steroidal Anti-inflammatories (NSAIDs)
- Having a chat to your GP about the use of NSAIDs is another step you can take in an attempt to reduce the inflammation and therefore compression of the nerve root. This can also reduce your symptoms and possibly aid in a quicker recovery.
- Self neural glides (Neural Mobilisations)
- Neural mobilisations improve homeostasis of the nervous system via mobilising neural structures and their surroundings through manual techniques or exercise (1). The effects of this include the reduction of swelling, a reduction of thermal/mechanical pain and a production of intraneural fluid (1).
- A qualified physiotherapist is able to do this in a safe and stable manner with that has been clinically proven to provide significant benefits in both pain and function (2). However, a self “glider” if done correctly can also achieve improvements in these areas.
- Which glider to use depends upon which disc is injured and therefore which nerve root is irritated. Once the nerve is determined by a health professional and/or confirmed by an x-ray, CT or MRI – they can educate you on how to perform these in a safe manner. The link below shows the tests used to determine which nerve is injured and how to perform a glider yourself. The video below shows a neural glide exercise for those with lumbar radiculopathy.
Cervical Neural Gliders
LUMBAR SPINE NEURAL GLIDE
Strengthening
-
- Another proven method of management for cervical radiculopathy is strengthening. However, determining which strengthening exercises are appropriate for you and your condition is dependent upon a range of factors and should be evaluated and prescribed by a qualified health professional.
- Strengthening weakened areas can help improve recovery from and prevention of radiculopathy.
- Some generic focus areas for cervical radiculopathy include the cervical extensors, deep neck flexors and upper trapezius.
- For lumbar radiculopathy – strengthening exercises that target your core and gluteal muscles can help improve stability and position of the lower back and in turn reduce these lower leg symptoms.
Strengthening examples: Anti-gravity neck holds + arm lifts (Cervical)


Single leg bridges with theraband (Lumbar) Core exercise: Bird Dog (Lumbar)


What OTHERS can do:
- Physiotherapy
- Both strengthening and neural mobilisations are areas physiotherapists are adept in prescribing and performing to improve pain function in radiculopathy clients. Beside these, physiotherapists can also apply manual therapy techniques such as traction and mobilisations. Research shows that when manual therapy is used in conjunction with exercise – improvements in client’s movement, pain and disability are gained (2).
- Corticosteroid injection or surgery
- If conservative methods such as rest, ice, NSAIDs and physiotherapy/strengthening provide little or no benefit then other options may be considered.
- A meta-analysis involving a number of studies concluded surgery showed the greatest improvement of pain – while corticosteroids were also found to be effective in reducing pain in a substantial portion of clients (5). Placebo treatments were also included within the studies and the lack of improvement in these groups further supported their findings (5).
If you are experiencing neck or lower back pain with or without referral into the arms or legs, it is important to see your GP or book an appointment with a qualified health professional. If you have any questions or want to book an appointment with POGO, feel free to contact us – details in the link below. https://www.pogophysio.com.au/contact-us/

Alec Lablache POGO Physiotherapist
Featured in the Top 50 Physical Therapy Blog
References
- Basson, A., Olivier, B., Ellis, R., Coppieters, M., Stewart, A., & Mudzi, W. (2017). The effectiveness of neural mobilization for neuromusculoskeletal conditions: A systematic review and meta-analysis. The Journal of Orthopaedic and Sports Physical Therapy, 47(9), 593-615. doi:10.2519/jospt.2017.7117
- Boyles, R., Toy, P., Mellon, J., Hayes, M., & Hammer, B. (2011). Effectiveness of manual physical therapy in the treatment of cervical radiculopathy: A systematic review. Journal of Manual & Manipulative Therapy, 19(3), 135-142. doi:10.1179/2042618611Y.0000000011
- Ellis, R. F., & Hing, W. A. (2008). Neural mobilization: A systematic review of randomized controlled trials with an analysis of therapeutic efficacy. Journal of Manual & Manipulative Therapy, 16(1), 8-22. doi:10.1179/106698108790818594
- Savva, C., & Giakas, G. (2012;2013;). The effect of cervical traction combined with neural mobilization on pain and disability in cervical radiculopathy. A case report. Manual Therapy, 18(5), 443-446. doi:10.1016/j.math.2012.06.012
- Zhang, X., Zhang, Z., Wen, J., Lu, J., Sun, Y., & Sang, D. (2018). The effectiveness of therapeutic strategies for patients with radiculopathy: A network meta-analysis. Molecular Pain, 14, 1744806918768972. doi:10.1177/1744806918768972