Arthrogenic Muscle Inhibition – Knee Joint Injuries
What is Arthrogenic Muscle Inhibition?
Arthrogenic Muscle Inhibition (AMI) is a common neuromuscular impairment that occurs following knee joint surgery, injury or pain. AMI could be thought of as the body’s protective ‘off-switch’. It is characterised by quadriceps inhibition, where the body attempts to shield the joint from further injury or aggravation (Kim, 2024). AMI is a frustrating roadblock for both practitioners and clients and is incredibly important to address in knee joint rehabilitation.
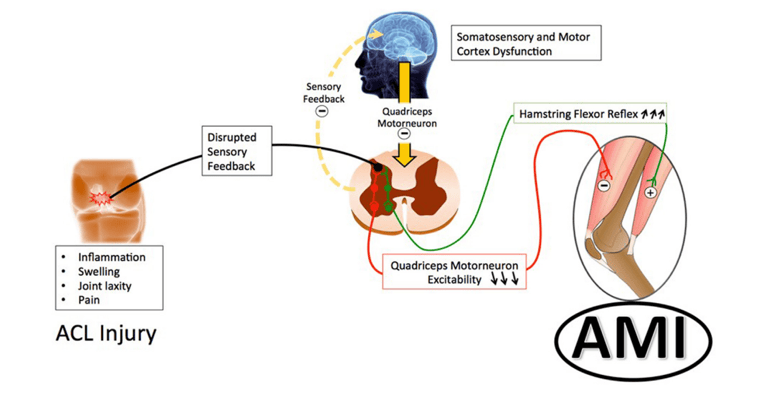
- AMI is driven by three main neurophysiological mechanisms that, in conjunction, contribute to quadriceps inhibition:
- Local: Swelling, stiffness, structural damage and pain inhibits sensory feedback from the joint directly
- Spinal: Reduced sensory feedback from the joint alters the excitability of reflex pathways in the spinal cord (E.g Flexion reflex which increases hamstring contracture) (Rice & McNair, 2009)
- Cortical: Inhibition & reduced excitation from the brain directly, limiting voluntary muscle activation (Forelli, 2025)
Who is affected by AMI?
AMI is most commonly seen and documented in acute knee joint injury, pathology or post operatively (Sonnery-Cottet, 2022).
Following knee surgery, recent research has shown that 36% of patients continued to show signs of AMI 2-weeks post operatively (Le Guen, 2025). Following ACL reconstruction, additional literature has identified 56% of patients displayed AMI in their first appointment following surgery (Sonnery-Cottet, 2022). In these acute settings, localised swelling and pain are the main driving factors of AMI. Longer term, however, research has shown that AMI can persist for months or even years following more complex knee joint injuries where more than one structure is damaged (e.g ACL + meniscus injury) (Rice & McNair, 2009; Sonnery-Cottet B. , 2022).
Without addressing AMI in the acute injury phase, poor rehabilitation outcomes become more likely. Altered gait mechanics, lean muscle mass deficits, long-term strength asymmetries and reduced agility capacity are examples of long-term consequences (Forelli, 2025).
Assessing & Classifying AMI
If you’ve ever had a knee injury or surgery and noticed it to be more challenging to contract or feel your quadriceps when trying to straighten your knee, during exercise or daily activity, it is likely a result of AMI. A simple assessment tool, based on the SANTI Classification can effectively identify severity of AMI (Le Guen, 2025):
- Grade 0: Normal VMO contraction
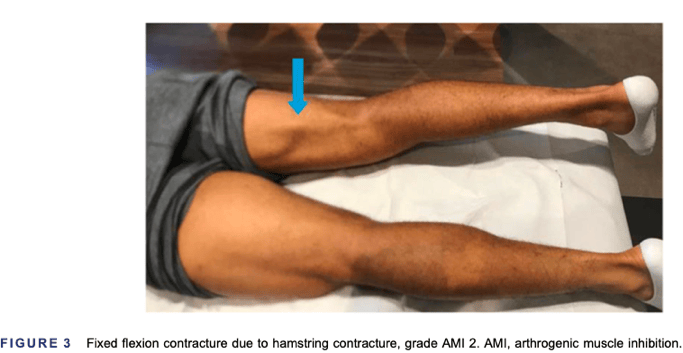
- Grade 1: VMO contraction inhibited with no knee extension deficit
- Grade 2: VMO contraction inhibited with associated knee extension deficit due to hamstring contracture
- Grade 3: Passive chronic extension deficit due to posterior capsular retraction
 (Le Guen, 2025)
(Le Guen, 2025)
Rest assured, there are rehabilitation exercises and techniques that can be implemented to reduce the effects of AMI and improve quadriceps activity following knee injury or surgery.
Overcoming AMI: Exercise & Rehabilitation Recommendations
Persistent or un-addressed AMI can cause a delay in rehabilitation progression and be the cause of ongoing knee pain. In the acute phases, research describes benefit in the following rehabilitation methods to reduce the effects of AMI.
Electromagnetic Muscle Stimulation (EMS) – e.g TENS, COMPEX
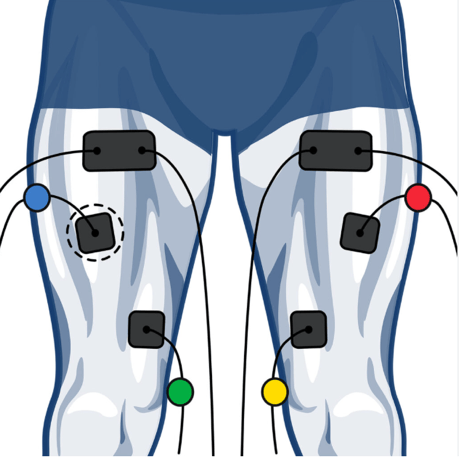 Provides direct muscle stimulation through surface electrodes without the requirement for active muscle contraction and without joint load (Forelli, 2025; Rush, 2021)
Provides direct muscle stimulation through surface electrodes without the requirement for active muscle contraction and without joint load (Forelli, 2025; Rush, 2021)- The benefit here is that you can bypass spinal & cortical AMI and provide direct muscle stimulus
Cryotherapy
- Application of ice has been shown to reduce swelling and pain, thus mitigating local factors that contribute to AMI (Forelli, 2025; Rush, 2021)
Isometric Exercises
- Isometric exercises are performed by holding a certain position for time (e.g Wall Sit, Leg Press Holds; Supine Knee Extension Holds).
- Isometrics allow muscle loading in comfortable joint positions, increase proprioception and quadriceps activation (Forelli, 2025)
Neuromuscular Control Exercises
Exercises that involve balance, coordination and dual-task training in later stage rehabilitation have been correlated to a 15% improvement in limb symmetry during sport specific tasks (Forelli, 2025)
Blood Flow Restriction (BFR)
BFR training allows a high muscle stimulus with minimal joint loading and has shown strength improvements of up to 25% in 6-8 weeks (completed 3/wk) (Benjaminse, 2006)
Structuring a Rehabilitation Session – Anecdotal Commentary
The task of structuring a rehabilitation session when knee pain persists as a result of AMI can be challenging as a practitioner. The reality that you need to increase quadriceps strength of the client, however knee pain limits extensive loading of this region, is a common hurdle that must be overcome in order to yield positive physiological adaptation. As a client, AMI can be extremely frustrating when not appropriately addressed.
In the art vs science of exercise prescription, an appropriate warm up can be extremely beneficial in clients with AMI. It may even be the difference between a successful rehabilitation session where quadriceps loading and is tolerated without knee pain, and a session that is limited by discomfort. Incorporating exercise modalities such as the Bike, Leg Press Holds or Isometric Terminal Knee Extensions may provide a tolerable stimulus that increases quadriceps proprioception and reduces AMI prior to the main exercises of the session such as split squats or leg extensions.
The following prescription may be useful:
Bike:
- Heavy Resistance – 7-8/10 RPE
- 5mins
Leg Press Holds – 60-90deg:
- Moderate Resistance – 7/10 RPE
- 4x 30sec
Floor Seated Terminal Knee Extensions:
- Concentration during movement is key – 6/10 RPE
- 3x [3x 10sec Holds]
Key Takeaways
- AMI is a common neuromuscular impairment following ACL Reconstruction or other Knee Surgery
- Thought of as the body’s protective “off switch”, AMI is characterised by quadriceps inhibition.
- Local, Spinal and Cortical factors contribute to AMI.
- AMI is most present in early rehab phases (0-4 weeks) but can last for months to years following ACLr
- Research has shown that Electromagnetic Muscle Stimulation, Cryotherapy and Exercise
- Rehabilitation are effective at mitigating the effects of AMI.
- Appropriate session structure & warm up can be missing link that provides a successful rehabilitation session without knee pain and high quadriceps load tom improve adaptation.
Lachie Adams
Exercise Physiologist
Bibliography
Benjaminse. (2006). Clinical Diagnosis of an Anterior Cruciate Ligament Rupture: A Meta-Analysis. Journal of Orthopaedic Sports Physical Therapy.
Forelli, F. (2025). Rethinking the Assessment of Arthrogenic Muscle Inhibition After ACL Reconstruction: Implications for Return-to-Sport Decision-Making—A Narrative Review. Journal of Clinical Medicine.
Kim, M. (2024). Assessment of arthrogenic quadriceps muscle inhibition by physical examination in the supine position during isometric contraction is feasible as demonstrated by electromyography: a cross-sectional study. Journal of Orthopaedic Surgery and Research.
Le Guen, A. (2025). Arthrogenic muscle inhibition: A prevalent issue in knee arthroplasty. Knee Surgery, Sports Traumatology, Arthroscopy.
Le Guen, A. (2025). Clinical SANTI classification of arthrogenic muscle inhibition has an excellent inter-rater and intra-rater reliability in preoperative and post-operative anterior cruciate ligament rupture. Knee Surgery, Sports Traumatology, Arthroscopy.
Rice, D., & McNair, P. (2009). Quadriceps Arthrogenic Muscle Inhibition: Neural Mechanisms and Treatment Perspectives. Seminars in Arthritis and Rheumatism.
Rush, J. (2021). Understanding Athletic Trainers’ Knowledge, Intervention, and Barriers Toward Arthrogenic Muscle Inhibition. Journal of Sport Rehabilitation.
Sonnery-Cottet. (2022). Arthrogenic Muscle Inhibition Following Knee Injury or Surgery: Pathophysiology, Classification, and Treatment. Video Journal of Sports Medicine.
Sonnery-Cottet, B. (2022). Prevention of knee stiffness following ligament reconstruction: Understanding the role of Arthrogenic Muscle Inhibition (AMI). Orthopaedics & Traumatology: Surgery & Research.