A look at SIJ FAQ’s with Lindsay Young
As a physiotherapist I often field questions relating to the SIJ (sacroiliac joint) and in particular sacroiliac joint pain. In this post I look at the most frequently asked questions that I receive.
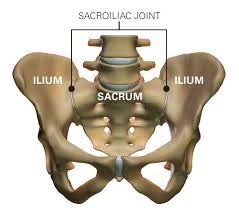
What is the SIJ?
The SIJ (sacroiliac joint) is where the lumbar spine/lower back joins to the pelvis. Its role is transfer load from the lumbar spine to the lower limb. Because of its role the SIJ is an inherently stable joint as its surface is made of irregular bony shapes that fit together like a jigsaw. It is then reinforced well by a system of ligaments and muscles. The SIJ has only a small amount of movement, roughly 5 degrees or 2-4mm in any direction. This movement is commonly termed nutation and counter-nutation.
Injury or pain in the SIJ
SIJ pain is overly diagnosed and is often mistaken for lower back pain because of referral to the area. A recent study in Australia found that 71% of women develop lumbo-pelvic pain during pregnancy and 8-15% of these suffers become chronic. Besides pregnancy SIJ disorders will usually only develop after direct trauma to the area.
People suffering SIJ problems will often report:
- pain and difficulty with sitting and/or standing
- moving from sitting to standing
- standing on one leg (eg to put pants on)
- walking, jumping, jogging
- rolling in bed
- getting in and out of the car
- driving
Why does the area get sore during pregnancy?
It was originally thought that the hormone relaxin that causes increased ligament laxity to the SIJ is responsible for SIJ pain during pregnancy. It is not possible to measure accurately the movement of the SIJ during pregnancy as the radiological studies required can harm the baby. Recent studies however have found that there is no link between relaxin levels and pelvic girdle pain, disability or pain provocation tests. Hormone levels however may play a role in increasing sensitivity and perception of pain during pregnancy. The increased weight of the baby, increased ligament laxity and decreased abdominal support in the area will also play a role in causing abnormal movement patterns and poor posturing.
The myths around SIJ pain
For years various therapists have been diagnosing clients with instability problems where the SIJ does not more enough, moves too much, or is “out of position”. There is however very little conclusive evidence around any of these theories, and any attempt by therapists to measure SIJ motion with their own hands has been proven to have poor reliability. Studies of clients who have suffered chronic SIJ pain have also showed increased activation and muscle tightness of some core muscles dispelling the myth that core-stability is the cure.
But what if having physio helps my pain?
Don’t stress there is still a role for hands on physiotherapy. If massage, acupuncture, joint mobilisation, helps reduce muscle tightness and pain it is indicated in the early stages of pain disorders with the goal to be providing the client with pain relief and reducing fear of movement. Simply put if hands on treatment does not reduce pain it is probably not appropriate. What practitioners need to be careful of is statements like putting your “SIJ joint back out” as this often causes fear avoidant behaviours in clients.
How can my physiotherapist determine if I have SIJ Pain?
Your physiothearpist will conduct a series of tests that first rule out the lumbar spine as a source of pain. There are then five tests that can be carried out and for a diagnosis of SIJ pain three out of the five need to be positive.
These tests include the:
- Sacral thrust (posterior to anterior pressure) test
- Thigh thrust (anterior to posterior pressure) test
- Torsion test (hip flexion of one leg and extension of the other)
- Distraction test
- Compression test
Don’t confuse SIJ with sacroilitis!
Sacroilitis is inflammation of the SIJ and it’s pain is often made worse with compression. Alternately in pelvic girdle pain disorders, the pain is often relieved with compression. Sacroilitis is typically present in inflammatory arthritic conditions and often needs a blood test, MRI and a rheumatologist to diagnose to disease.
So how do physiotherapists treat SIJ pain?
Well, it is not that simple. There is no one size fits all solution. Each client needs to be assessed for all the cognitive, emotion and physical contributory factors and then suitable treatment and management plans should be put in place.
Some of the cognitive contributing factors include:
- Poor belief patterns around pain
- bad lifestyle habits
- fear around movement
- stress and anxiety
- Lack of coping mechanisms
- Boom-bust type activity levels
- Lack of support
Some of the functional (physical) factors include:
- Poor movement patterns and postures
- Lack of exposure to aggravating load
- Lack of meaningful activity such as participating in sports you enjoy
How long does rehabilitation of SIJ disorders take?
Once again there is no way of predicting how long it will take a client to recover from an episode of SIJ pain. It is often however not a quick process, especially in chronic cases as often the contributing factors have become engrained in peoples lifestyles. With good management however clients should be able to notice changes to their pain in the first couple of weeks and start seeing large changes to function in 3-6 months.
Some things your physiotherapist might recommended you do to help you SIJ pain include:
- Increased activation in activities that bring meaning to your life
- Counselling or psychology
- Medication to control pain and reduce fear avoidant behaviours
- Increased general physical activity (walking, swimming…etc)
- Clinical pilates to change poor movement patterns and address muscle imbalances
- Hydrotherapy
What if conservative management fails?
There are cases where even the best conservative management is not enough to reduce pain to a bearable or functional level. In these instances the first step is injection of a cortico-steroid (anti-inflammatory) or PRP injections (platelet rich plasma) may be indicated. There is clinically little evidence thus far to support these injections as a treatment of SIJ pain but in certain circumstances they could be used.
What about surgery?
Surgical management of the SIJ involves fusion of the joint. This is an absolute last resort and is a highly controversial option. It is only indicated in very severe cases of high pain and disability of greater than 6 months and when the client is fully aware of the potential outcomes of the surgery. Like all spinal surgery an SIJ fusion carries with it risks of nerve damage and increases in pain and disability.
I hope this review of SIJ pain answers a few key questions that you have around SIJ pain and SIJ disorders.
Lindsay Young (APAM)
Physiotherapist
References
Beales, Darren, and Peter O’Sullivan. ‘Sacroiliac Joint- Pelvis Series’. Sacroiliac Joint- Pelvis Series. N.p., 2015. Web. 1 Nov. 2015.
Mayoclinic.org,. ‘Sacroiliitis – Mayo Clinic’. N.p., 2015. Web. 4 Nov. 2015.
Dionne, Cassie. ‘Why Your SI Joint Is Such A Pain (And 4 Exercises To Fix It)’. Breaking Muscle. N.p., 2015. Web. 4 Nov. 2015.
Dall, B. E., Eden, S. V., & Rahl, M. D. (Eds.). (2014). Surgery for the Painful, Dysfunctional Sacroiliac Joint: A Clinical Guide. Springer.
Braun, J., Bollow, M., Eggens, U., König, H., Distler, A., & Sieper, J. (1994). Use of dynamic magnetic resonance imaging with fast imaging in the detection of early and advanced sacroiliitis in spondylarthropathy patients. Arthritis & Rheumatism, 37(7), 1039-1045.








Good written blog for The SIJ is where the lumbar spine/lower back joins to the pelvis.
Thank you.
b.beer@pogophysio.com.au
Brad Beer
Well written Brad. I appreciate the effort of sharing your thoughts about SIJ. Mostly patient who has symptoms but does not know what to do. Too late to consult physiotherapist is not a good idea.
Thanks for your comments.
Regards Brad Beer